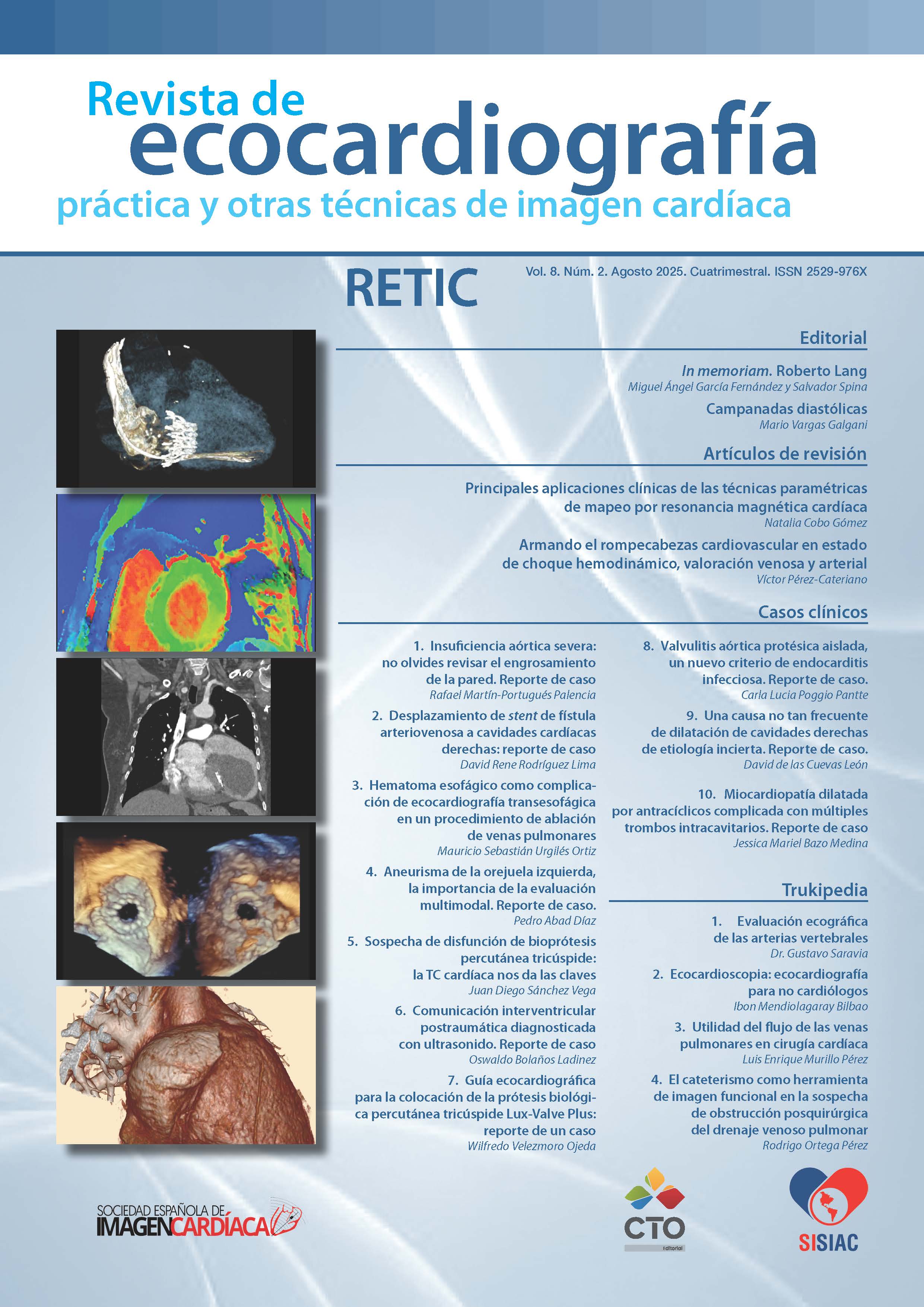
Main clinical applications of parametric cardiac magnetic resonance mapping techniques
DOI:
https://doi.org/10.37615/retic.v8n2a2Keywords:
mapping, magnetic resonance, cardiomyopathyAbstract
Parametric mapping techniques provide a non-invasive tool for quantifying tissue alterations in various cardiac pathologies. They measure changes in myocardial composition based on T1, T2, and T2* (star) relaxation times and extracellular volume. These techniques focus on specific pathological pathways, which are primarily related to intracellular alterations in the cardiomyocyte and/or extracellular alterations in the myocardial interstitium. This improves the diagnosis, risk stratification, follow-up and assessment of treatment response for various types of cardiomyopathies.
This article shows the main clinical scenarios in which these parametric techniques are applied.
Downloads
Metrics
References
Messroghli DR, Moon JC, Ferreira VM, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2 T2* and extracellular volume: A consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovascular Magn Reson (2017); 19 (1):75. DOI: https://doi.org/10.1186/s12968-017-0389-8
Haaf P, Garg P, Messroghli DR, Broadbent DA, et al. Cardiac T1 Mapping and Extracellular Volume (ECV) in clinical practice: comprehensive review. J Cardiovasc Magn Reson. 2016;18(1):89. DOI: https://doi.org/10.1186/s12968-016-0308-4
Captur G, Manisty C, Moon JC. Cardiac MRI evaluation of myocardial disease. Heart. 2016;102(18):1429–35. DOI: https://doi.org/10.1136/heartjnl-2015-309077
Lewis AJM, Burrage MK, Ferreira VM. Cardiovascular magnetic resonance imaging for inflammatory heart diseases. Cardiovasc Diagn Ther. 2020; 10(3): 598-609. DOI: https://doi.org/10.21037/cdt.2019.12.09
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer cm, Carbone I, Sechtem U, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: Expert recommendations. J am Coll Cardiol. 2018; 72 (24)3158-76. DOI: https://doi.org/10.1016/j.jacc.2018.09.072
Ntusi NAB, Piecnik SK, Francis JM et al. Diffuse myocardial fibrosis and inflammation in rheumatoid arthritis: Insights from CMR T1 mapping. JACC Cardiovasc Imaging 2015;8(5):526-36. DOI: https://doi.org/10.1016/j.jcmg.2014.12.025
Guo Q, Wu L-M, Wang Z, et al. Early detection of silent myocardial impairment in patients with new onset drug-naive systemic lupus erythematosus. A three-center prospective study (myocardial impairment in new onset SLE): A three- center prospective study. Arthritis Rheumatol 2018;70(12):2014-24. DOI: https://doi.org/10.1002/art.40671
Argentiero A, Carella MC, Mandunzio D, et al. Cardiac magnetic resonance as risk stratification tool in non- ischemic dilated cardiomyopathy referred for implantable cardioverter defibrillator therapy – state of art and perspectives. J Clin Med 2023;12(24):7752. DOI: https://doi.org/10.3390/jcm12247752
Pan JA, Kerwin MJ, Salerno M. Native T1 mapping, extracellular volume mapping, and late gadolinium enhancement in cardiac amyloidosis: A meta-analysis. JACC Cardiovasc Imaging 2020;13(6):1299–310. DOI: https://doi.org/10.1016/j.jcmg.2020.03.010
Cai S, Haghbayan H, Chan KKW, et al. Tissue mapping by cardiac magnetic resonance imaging for the prognostication of cardiac amyloidosis: A systematic review and meta-analysis. Int J Cardiol 2024;403(131892):131892. DOI: https://doi.org/10.1016/j.ijcard.2024.131892
Ponsiglione A, Gambardella M, Green R, et al. Cardiovascular magnetic resonance native T1 mapping in Anderson-Fabry disease: a systematic review and meta-analysis. J Cardiovasc Magn Reson 2022;24(1):31. DOI: https://doi.org/10.1186/s12968-022-00859-z
Sado DM, White SK, Piechnik SK, et al. Identification and assessment of Anderson-Fabry disease by cardiovascular magnetic resonance noncontract myocardial T1 mapping. Circ Cardiovasc Imaging. 2013;6(3):392–8. DOI: https://doi.org/10.1161/CIRCIMAGING.112.000070
Swoboda PP, McDiarmid AK, Erhayiem B, et al. Assessing myocardial extracellular volume by T1 mapping to distinguish hypertrophic cardiomyopathy from athlete’s heart. J Am Coll Cardiol. 2016;67(18):2189–90. DOI: https://doi.org/10.1016/j.jacc.2016.02.054
Plana JC, Thavendiranathan P, Bucciarelli-Ducci C, Lancellotti P. Multi-modality imaging in the assessment of cardiovascular toxicity in the cancer patient. JACC Cardiovasc Imaging 2018;11(8):1173–86. DOI: https://doi.org/10.1016/j.jcmg.2018.06.003
Lisi C, Catapano F, Rondi P, et al. Multimodality imaging in cardio-oncology: the added value of CMR and CCTA. Br J Radiol 2023;96(1150):20220999. DOI: https://doi.org/10.1259/bjr.20220999
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Natalia Cobo Gómez, Jordi Broncano Cabrero, Gabriela Muller Bravo, Antonio Luna Alcalá

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
RETIC is distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) license https://creativecommons.org/licenses/by-nc-nd/4.0 which allows sharing, copying and redistribution of the material in any medium or format, under the following terms:
- Attribution: you must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests that the licensor endorses you or your use.
- Non-commercial: you may not use the material for commercial purposes.
- No Derivatives: if you remix, transform or build upon the material, you may not distribute the modified material.
- No Additional Restrictions: you may not apply legal terms or technological measures that legally restrict others from doing anything permitted by the license.